One of the most common gastric afflictions in America is the stomach ulcer. Long thought to be caused by stress, alcoholism, spicy food or a combination of the three, understanding the real cause of ulcers has recently made them easier to recover from and prevent.
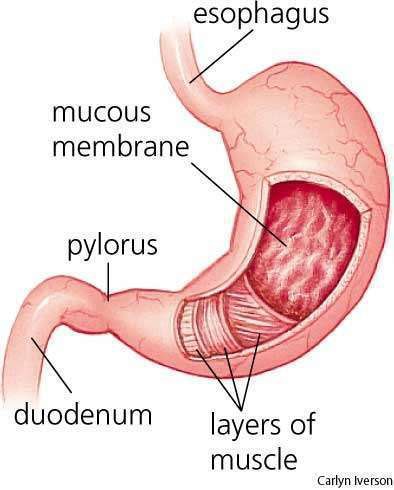
Peptic ulcers are holes or breaks in the protective lining of the duodenum (the upper part of the small intestine) or the stomach, both areas that come into contact with stomach acids and enzymes. Duodenal ulcers are more common than stomach ulcers. Comparatively rare are esophageal ulcers, which form in the esophagus — or swallowing tube — and are often a result of alcohol abuse.
Approximately 500,000 new cases of peptic ulcer are reported each year. At any given time, as many as 5 million people are affected in the United States alone. Ninety to one hundred percent of the duodenal ulcers, and 70 percent of the gastric ulcers, throw a positive for H. pylori bacteria in blood and saliva tests when the patient is diagnosed with ulcers. While excessive stomach acid secretion certainly plays a role in the development of ulcers, a relatively recent theory holds that bacterial infection is the primary cause of peptic ulcers.
The remaining numbers of those diagnosed are heavily attributed to overuse of over-the-counter painkillers (such as aspirin, ibuprofen, and naproxen), heavy alcohol use and smoking, as all three exacerbate and may promote the development of ulcers. Research indicates heavy smokers are more prone to developing duodenal ulcers than are nonsmokers, and daily use of painkillers is proven to cause peptic damage.
People who have a family history of ulcers seem to have a greater likelihood of acquiring the condition, as do people with type O blood. (Forty-five percent of people in the U.S. have Type O-positive or -negative blood.) In addition, liver disease, rheumatoid arthritis and emphysema are among the conditions that may increase vulnerability to ulcers. Stomach and pancreatic cancers also can cause these sores to form.
|
ULCER TREATMENTS | Relieving the irritation that comes with ulcers is key to enabling healing to progress naturally. Antacids counteract stomach acid and relieve symptoms, but they can also cause complications. For example, sodium bicarbonate, a primary antacid ingredient, contains large amounts of sodium, which can aggravate kidney disease or high blood pressure. Johns-Hopkins Medical Journal suggests a balanced regimen of both homeopathic and mainstream treatments for the best results. There are many natural remedies and cures suggested, but a few are mentioned in more than one reputable medical journal as tried-and true alternatives to over-the-counter medications offering palliative relief for ulcer pain and discomfort. Raw honey soothes and reduces inflammation of the lining of the stomach and is good for healing as well. Garlic’s antibacterial properties include fighting H. pylori. Taking (orally) two small crushed cloves a day has shown to be effective in killing bacteria and healing ulcers. Plums and other red and purple colored foods such as berries inhibit the growth of H. pylori. The less bacteria present, the lower the chance for lesions forming. Recently, endoscopic cautery (burning of tissue through an endoscope), direct injection of medications, and lasers have been quite successful in stopping bleeding, reducing the size of lesions, and correcting strictures (scar formation caused by lesions). These procedures have spared many individuals from the danger of actually having to cut into the gut to get to the ulcer. With proper diagnosis and treatment, the outcome is rarely surgery related. |
Diagnosis is critical, and necessary tests to determine the presence of H. pylori are often overlooked. Most positive cases can be cured with a combination of antibiotics and acid-blocking drugs or bismuth subsalicylate (better known as Pepto Bismol). Unfortunately, even though this information has been widely disseminated in medical journals, some doctors still send ulcer patients home with little more than orders to take it easy, knock off the booze, and eat a bland diet. If you have ulcer-like symptoms, ask your doctor to perform tests that can determine whether you have the actual bacteria present, so if prescription medications are appropriate for your condition, you get them.
In extreme cases, surgery is appropriate for ulcers that recur or are life-threatening, such as perforated ulcers. Sometimes, surgeons remove a portion of the stomach and parts of the vagus nerve (which controls digestive secretions) to reduce stomach acid production. Usually, ulcers do not reappear after surgery.
Knowing when to say when is important. A constant, aggravating pain that resembles hunger pangs is one extremely prevalent symptom. Others include epigastric distress 45-60 minutes after meals and/or nocturnal pain, tenderness in the gut or blood in the stool. A combination of any of these symptoms is plenty of reason to go to the doctor to have some tests. Treatment is generally successful in 6-8 weeks. You don’t have to live with the pain and discomfort of ulcers anymore.











